Bladder lesions are abnormal growths or tumours on the bladder lining. They can be removed by having an operation called a transurethral resection of bladder tumour (TURBT), although treatment options depend on the size of the tumour, where it is located and how far the cancer may have spread.
We treat every patient as an individual and your care will be tailored specifically to your needs. Our expert consultants will be with you every step of the way on your treatment journey.
Why you might need it
Bladder cancer develops when there is a growth of abnormal tissue in the lining of the bladder (the organ that stores urine in the body). Sometimes the abnormal tissue, known as a tumour, can spread into the muscles surrounding the bladder.
The most common symptom of bladder cancer is blood in the urine, however an urgent and frequent need to urinate and a burning sensation when passing water are also symptoms of bladder cancer. It is important to see your GP if you experience any of these symptoms, which can also be related to more common conditions including cystitis, kidney stones or an enlarged prostate (in men).
TURBT (together with chemotherapy or immunotherapy) is the main treatment option for early bladder cancer that hasn't spread. Surgical removal of the bladder may be required for later stage (and more invasive) bladder cancer.
We pride ourselves on our clinical excellence, you'll be looked after by an experienced multi-disciplinary care team.
How much does Bladder lesion removal cost at Spire Edinburgh Hospitals Murrayfield and Shawfair Park
We can't display a fee for this procedure just now. Please contact us for a quote.
Who will do it?
Our patients are at the heart of what we do and we want you to be in control of your care. To us, that means you can choose the consultant you want to see, and when you want. They'll be with you every step of the way.
All of our consultants are of the highest calibre and benefit from working in our modern, well-equipped hospitals.
Our consultants have high standards to meet, often holding specialist NHS posts and delivering expertise in complex sub-specialty surgeries. Many of our consultants have international reputations for their research in their specialised field.
Before your treatment
You will have a formal consultation with a healthcare professional. During this time you will be able to explain your medical history, symptoms and raise any concerns that you might have.
We will also discuss with you whether any further diagnostic tests, such as scans or blood tests, are needed. Any additional costs will be discussed before further tests are carried out.
Preparing for your treatment
We've tried to make your experience with us as easy and relaxed as possible.
For more information on visiting hours, our food, what to pack if you're staying with us, parking and all those other important practicalities, please visit our patient information pages.
Our dedicated team will also give you tailored advice to follow in the run up to your visit.
The procedure
We understand that if you're attending hospital for a TURBT this is probably a time of anxiety and worry for you. Our experienced and caring medical staff will be there for you, holding your hand, every step of the way.
TURBT is usually done under general anaesthesia. This means you will be asleep during the operation and will feel no pain.
Once the anaesthetic has taken effect, a thin rod-like instrument with a tiny light and lens on the tip, called a cystoscope, will be carefully inserted into the urethra (the tube that carries urine out of the body). Saline solution (salt water) will be passed through the cystoscope to fill the bladder up and to make the whole of the lining visible.
Your surgeon will find the lesion and insert a special wire loop through the cystoscope. An electric current is passed down the wire loop and used to cut or burn off the lesion. This also seals the wound to stop any bleeding. Some healthy tissue around the lesion may also be removed.
At the end of the procedure, the cystoscope is taken out and a catheter (a thin flexible tube) is passed into the urethra and left in place for about 24 hours. The catheter will drain urine from your bladder into a bag. The catheter may also be connected to a system which washes any blood and blood clots out of your bladder. This is called bladder irrigation.
The removed lesions are sent to a laboratory for examination. If the bladder lesion is cancerous, the tests will show how far the cancer has spread and if further treatment is required. In some cases, removing the lesion is all that is needed.
The procedure usually lasts 30 minutes, slightly longer if more than one lesion is present.
Aftercare
You should plan on spending the night in hospital with us. After the procedure, you will be taken from the operating theatre to a recovery room, where you will come round from the anaesthesia under close supervision.
After this, you will be taken to your room or comfortable area where you can rest and recuperate until we feel you’re ready to go home.
To ensure any remaining abnormal cells are killed and to help lower the chance of new lesions or tumours forming, you may be given anti-cancer drugs through the catheter. Giving drugs directly into the bladder means very little is absorbed into the rest of the body and so there are fewer side-effects.
The catheter will be removed before you go home.
Your friends and family will be able to visit pretty much anytime you want – we have flexible visiting hours.
Pain relief
If you are sore you may require painkillers and you may be given antibiotics to help prevent infection.
We will provide you with a supply of all the medicines your consultant feels you need to take home with you after you've left hospital, up to 14 days. This may be at an additional cost to some patients.
Recovery time
Follow your surgeon’s advice about driving, returning to work, heavy lifting, sport and sexual activity. You should not drive until you feel you could do an emergency stop without discomfort. Eat plenty of vegetables, fruit and high fibre foods such as brown rice and wholemeal bread and pasta. This helps to avoid constipation, which may increase bleeding in the bladder. Your surgeon may prescribe a mild laxative for a few days.
Try to drink fluids regularly for a few weeks afterwards to help flush out any possible infection.
How your loved ones can help
Once you’re ready to be discharged, you’ll need to arrange a taxi, friend or family member to take you home because you won’t be able to drive. You should also ask them to help with shopping and cleaning for a few weeks.
Looking after you
We’re with you every step of the way through your recovery, even after you’ve left hospital.
We will provide you with all the appropriate medication, advice on what you should and shouldn't do, and any other follow-up support you need. The laboratory results are usually sent in a report to your consultant. Your consultant will review the results and discuss them with you at your follow-up appointment. The results will give a better understanding of your bladder problem and your consultant will offer suitable advice and treatment.
As with all medical treatments, complications following TURBT can occur but most people are unaffected. Your consultant will talk to you about the possible risks and complications of having this procedure. If you experience any of these symptoms don’t hesitate to call us:
- a burning sensation on passing urine or your urine becomes smelly
- increasing pain
- an inability to pass urine
- an increase in blood in the urine
- a high temperature or fever.
We will talk to you about the possible risks and complications of having this procedure and how they apply to you.
If you have any questions or concerns about your recovery, we're ready to help.
Why choose Spire?
We are committed to delivering excellent individual care and customer service across our network of hospitals, clinics and specialist care centres around the UK. Our dedicated and highly trained team aim to achieve consistently excellent results. For us it's more than just treating patients, it's about looking after people.
Important to note
The treatment described on this page may be adapted to meet your individual needs, so it's important to follow your healthcare professional's advice and raise any questions that you may have with them.
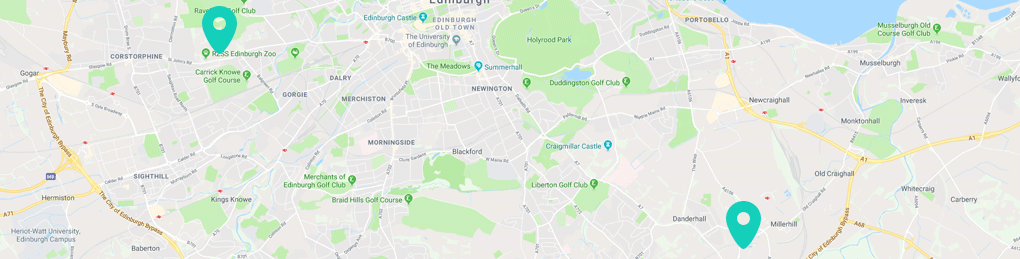
How to get to us
Spire Murrayfield is an approximate 20 minute drive from Edinburgh Airport or 10 minutes from Haymarket train station. Regular buses serve the area well. Spire Shawfair Park is located to the south east of the city centre close to the City Bypass and the Royal Infirmary at 10 Easter Shawfair, Edinburgh, EH22 1FE.
Spire Edinburgh Hospitals Murrayfield and Shawfair Park,
Spire Murrayfield Hospital
122 Corstorphine Road
Edinburgh
EH12 6UD