Hysterectomy surgery at Spire St Anthony's Hospital
Removal of the uterus and possibly also the ovaries and fallopian tubes.
Although it’s a major procedure, around 30,000 hysterectomies are carried out each year in the UK according to the NHS, mainly in women aged 40–50.
Sometimes also called
- Abdominal hysterectomy
- Laparoscopic hysterectomy
- Vaginal hysterectomy
A hysterectomy is an operation to remove the uterus (womb). Depending on why the surgery is needed it may also involve removing one or both of the fallopian tubes and one or both of the ovaries.
After the operation you won’t be able to have children and you won’t have any more periods. Although it’s a major procedure, around 30,000 hysterectomies are carried out each year in the UK according to the NHS.
Why you might need it
Women normally need to have a hysterectomy due to one of the following reasons, and where other treatment options have been unsuccessful:
- Heavy periods, which can often be caused by fibroids. These are non-cancerous tumours that grow in or around the womb.
- Endometriosis, a condition where cells that line the womb end up in other areas of the body and reproductive system, such as the ovaries, fallopian tubes, bladder and rectum.
- Pelvic inflammatory disease (PID), a bacterial infection of the female reproductive system. If detected early it can be treated with antibiotics. However, if it spreads, it can damage the womb and fallopian tubes, resulting in long-term pain.
- Adenomyosis, a common condition where the tissue that normally lines the inside of the womb starts to grow within its muscular wall.
- Prolapse of the uterus, where the tissues and ligaments that support the womb become weak, causing it to drop down from its normal position. Symptoms can include back pain, a feeling that something is coming down out of your vagina, leaking urine (urinary incontinence) and difficulty having sex. It can often occur as a result of childbirth.
- Ovarian cancer or cancer of the womb or cervix.
In some cases, removing the womb may be the only way of stopping the persistent heavy menstrual bleeding and pain that often accompanies these conditions.
If you decide to have the operation, your consultant will advise you on the options available most suitable for you:
- A vaginal hysterectomy involves removing the uterus (and fallopian tubes/ovaries if necessary) through the vagina and usually requires a hospital stay of 2 to 4 days.
- An abdominal hysterectomy involves removing the uterus (and fallopian tubes/ovaries if necessary) through a large cut on the abdomen and usually requires a hospital stay of 2 to 4 days.
- Laparoscopic hysterectomy involves making two or three small cuts to your abdomen, through which a tube like camera will be passed to enable your surgeon to view the uterus (womb). Special surgical instruments are then used to remove the uterus (and fallopian tubes/ovaries if necessary). This technique is less invasive resulting in smaller scars with a quicker recovery period to the traditional abdominal hysterectomy and requires a hospital stay of around 1 to 2 days.
If you have private medical insurance or are willing to pay for the operation yourself, we can help. You may be referred to one of our respected surgeons via your own GP. We will aim for you to see one our specialised consultants within a few days of your referral to us.
Pricing for Hysterectomy surgery at Spire St Anthony's Hospital
| Hysterectomy (abdominal) | |||
|---|---|---|---|
| Initial consultation [2] | £243 | ||
| Treatment price[3] | from £7,955 | ||
| Aftercare[4] | Included | ||
| Price[1] | from £8,198 | ||
|
Monthly treatment price (Loan applicable to the treatment cost and excludes the initial consultation) |
from £222 | ||
| Representative example | |
|---|---|
| Loan amount | £6,955 |
| Deposit | £1,000 |
| Loan period | 36 months |
| Representative APR | 9.9% |
| Total amount repayable | £7,992 |
| Hysterectomy (vaginal) | |||
|---|---|---|---|
| Initial consultation [2] | £290 | ||
| Treatment price[3] | from £8,570 | ||
| Aftercare[4] | Included | ||
| Price[1] | from £8,860 | ||
|
Monthly treatment price (Loan applicable to the treatment cost and excludes the initial consultation) |
from £242 | ||
| Representative example | |
|---|---|
| Loan amount | £7,570 |
| Deposit | £1,000 |
| Loan period | 36 months |
| Representative APR | 9.9% |
| Total amount repayable | £8,712 |
[1]The price shown is the ‘from price’ (ie the minimum cost of the procedure). Please note that for some procedures the actual price you are quoted may vary significantly and can increase depending on your choice of Consultant (who is an independent practitioner and not an employee of Spire). The fees charged by Consultants and Anaesthetists are set independently and are outside the control of Spire. The price may also vary depending on the type of anaesthetic, implant or drug used, and your medical history.
- [2]Initial Consultation” covers your initial appointment with your Consultant. The price displayed is a guide only as consultant fees may vary.
- [3]“Treatment” includes all the pre-assessment tests and the cost of the treatment, Consultant and Anaesthetist fees, nursing care, medication and food during your stay in hospital and any standard prosthesis. Your hospital stay is included as long as your Consultant advises is necessary.
- [4]“Aftercare” includes your care after you leave hospital, including consultations and physiotherapy visits (up to the number stated in your treatment letter), removal of stitches, change of dressings and the medication you need for up to 14 days after you leave hospital. Note that some home aids are not included.
Disclaimer
Spire Healthcare Limited is registered in England and Wales 1522532. Registered office: 3 Dorset Rise, London EC4Y 8EN. Spire Healthcare Limited acts as a credit broker and offers credit products from Omni Capital Retail Finance. Spire Healthcare Limited is authorised and regulated by the Financial Conduct Authority, registration number: 689975. Your application will be subject to a credit check using a recognised credit reference agency as part of our assessment process. Credit is subject to status, UK residents aged 18 years and over. For more information please visit https://www.omnicapitalretailfinance.co.uk/
Omni Capital Retail Finance Ltd finance options are subject to individual status and terms and conditions apply. Finance is provided by Omni Capital Retail Finance Ltd which is a credit intermediary. Spire Healthcare does not receive payment for introducing patients to lenders. All named here are authorised and regulated by the Financial Conduct Authority. Omni Capital Retail Finance Ltd is registered in England and Wales 7232938. Registered address: 10 Norwich Street, London, EC4A 1BD. Authorised and regulated by the Financial Conduct Authority, Firm Reference Number: 720279.
Spire St Anthony's Hospital can provide you with a single, fixed price for your procedure so there are no surprises. Please read Spire Healthcare's terms and conditions for full details of what’s included and excluded in your fixed price when paying for yourself. Finance options are available through our partner Omni Capital Retail Finance Ltd, 10 Norwich Street, London, EC4A 1BD.
Who will do it?
Our patients are at the heart of what we do and we want you to be in control of your care. To us, that means you can choose the consultant you want to see, and when you want. They'll be with you every step of the way.
All of our consultants are of the highest calibre and benefit from working in our modern, well-equipped hospitals.
Our consultants have high standards to meet, often holding specialist NHS posts and delivering expertise in complex sub-specialty surgeries. Many of our consultants have international reputations for their research in their specialised field.
Before your treatment
You will have a formal consultation with a healthcare professional. During this time you will be able to explain your medical history, symptoms and raise any concerns that you might have.
We will also discuss with you whether any further diagnostic tests, such as scans or blood tests, are needed. Any additional costs will be discussed before further tests are carried out.
Preparing for your treatment
We've tried to make your experience with us as easy and relaxed as possible.
For more information on visiting hours, our food, what to pack if you're staying with us, parking and all those other important practicalities, please visit our patient information pages.
Our dedicated team will also give you tailored advice to follow in the run up to your visit.
The procedure
We understand that having surgery can be a time of worry and anxiety. Our experienced and caring medical staff will be there for you, holding your hand, every step of the way.
You will be put under a general anaesthetic whichever procedure you have, so you’ll be asleep throughout.
During vaginal hysterectomy, your surgeon will make an incision to separate the vagina from the neck of the womb and remove the womb through the opening of the vagina.
The cut is sewn up using dissolvable stitches. This technique leaves no visible scars and usually takes about an hour. Alternatively, your surgeon may remove your womb with the help of a long, thin telescope (called a laparoscope), which enables them to see what is going on inside your belly.
Several small cuts are made in the skin on your abdomen and the laparoscope is inserted. Gas is pumped into the abdomen to inflate the space around your womb before your doctor removes it through the opening of the vagina. Again, dissolvable stitches are used to seal the cuts.
During abdominal hysterectomy, your surgeon will make either a vertical or horizontal incision on your abdomen and remove the womb through this long cut. Stitches or metal clips will be used to close the incision. The operation usually lasts about an hour.
Your surgeon will put in a catheter (tube) to drain urine from your bladder into a bag beside your bed because most women have difficulty passing urine for a few days after a hysterectomy.
Aftercare
After the procedure, you will be taken from the operating theatre to a recovery room, where you will come round from the anaesthesia under close supervision.
After this, you will be taken to your room or comfortable area where you can rest and recuperate until we feel you’re ready to go home.
A physiotherapist may visit you while you’re with us and show you some exercises to do that will help speed up your recovery.
Pain relief
You will feel sore after the operation and you may have some bruising and swelling, so we will give you pain relief medication while you’re with us.
We will provide you with a supply of all the medicines your consultant feels you need to take home with you after you've left hospital, up to 14 days. This may be at an additional cost to some patients.
Recovery time
A hysterectomy is a major operation. The length of your stay in hospital will depend on which type of procedure you had as well as your overall health and fitness.
If you have had a vaginal or laparoscopic hysterectomy, you probably won’t need to stay in for more than four nights. With an abdominal hysterectomy you're likely to be with us for 3-5 days.
It takes six to eight weeks to fully recover after an abdominal hysterectomy but it’s usually less after a vaginal or laparoscopy hysterectomy.
Whichever operation you have, you should take at least four weeks off work and rest as much as possible. You will be able to walk around after a day or two but don’t lift anything heavy or do any sporting activities until you’re fully recovered.
It’s important to do your physiotherapy exercises regularly, as this will help build your abdominal muscles back up. Your physio will probably also recommend you get back to walking and swimming once your wounds have healed.
Don't drive until you're comfortable wearing a seat belt – this could be up to eight weeks after surgery. Some car insurance companies require a certificate from your doctor stating that you are fit to drive.
Avoid sexual activity for at least six weeks and you might experience a temporary loss of interest in sex. This usually returns when you’re fully recovered and many women report that sexual activity and enjoyment actually improves after a hysterectomy.
Your surgeon will advise you when you can resume your normal activities. A full recovery can take up to 12 weeks.
If your ovaries were removed you may get menopausal symptoms such as hot flushes and vaginal dryness. Your doctor may recommend hormone replacement therapy to help with this.
How your loved ones can help
Once you’re ready to be discharged, you’ll need to arrange a taxi, friend or family member to take you home because you won’t be able to drive. You should also ask them to help with shopping and cleaning for a few weeks.
Looking after you
We’re with you every step of the way through your recovery, even after you’ve left hospital.
After your operation we will provide you with all the appropriate medication, physiotherapy exercises, advice on what you should and shouldn't do, and any other follow-up support you need. Typically your consultant will want to see you after your treatment to see how you’re doing and a follow up appointment will be made for you.
On rare occasions, complications following surgery can occur. The chance of complications depends on the exact type of operation you’re having and other factors such as your general health. Your consultant will talk to you about the possible risks and complications of having this procedure and how they apply to you.
If you have any questions or concerns we’re ready to help.
Why choose Spire?
We are committed to delivering excellent individual care and customer service across our network of hospitals, clinics and specialist care centres around the UK. Our dedicated and highly trained team aim to achieve consistently excellent results. For us it's more than just treating patients, it's about looking after people.
Important to note
The treatment described on this page may be adapted to meet your individual needs, so it's important to follow your healthcare professional's advice and raise any questions that you may have with them.
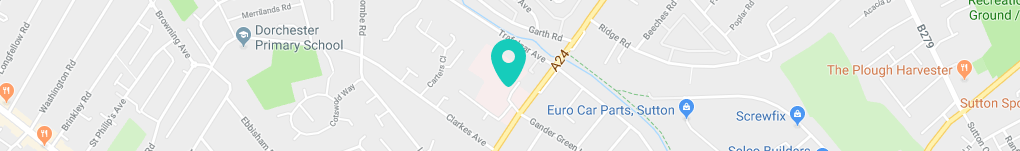
How to get to us
Spire St Anthony’s Hospital is a large private hospital providing an extensive range of treatments and services for our patients in Sutton and the surrounding Surrey and south London area.
Spire St Anthony's Hospital,
801 London Road
Cheam
Sutton
SM3 9DW