Haemorrhoids (piles) are very common and their symptoms can often disappear on their own after a few days. Sometimes though, these symptoms - such as itchiness, discharge, soreness and bleeding - are severe and don't go away. Haemorrhoid removal treatment is needed to treat them.
Why you might need it
You may have haemorrhoids because you have strained too hard when going to the toilet as a result of being constipated for a while. This could be because you don't have enough fibre in your diet.
Being overweight, pregnant or over 45, or having a family history of piles, can raise your risk of having haemorrhoids, according to clinical sources.
Your doctor may have suggested surgery because changing your diet, over-the-counter treatments and GP-prescribed medication have failed to get rid of your piles.
If you decide to have your treatment with us, you will be looked after by an experienced multi-disciplinary care team.
Haemorrhoids (or piles as they are commonly known) are generally an unspoken curse from which many of us suffer but are too embarrassed to discuss with our loved ones, let alone our GP. They are enlarged vascular ‘cushions’ found just inside or around the bottom (anus and lower rectum), thought to be caused by a variety of factors but commonly constipation, diarrhoea or excessive straining. They are common and it has been estimated that up to 50% of the population may suffer from symptomatic haemorrhoids at some point in their lives*.
How much does The Rafaelo Procedure cost at Spire St Anthony's Hospital
Who will do it?
Our patients are at the heart of what we do and we want you to be in control of your care. To us, that means you can choose the consultant you want to see, and when you want. They'll be with you every step of the way.
All of our consultants are of the highest calibre and benefit from working in our modern, well-equipped hospitals or clinics.
Our consultants have high standards to meet, often holding specialist NHS posts and delivering expertise in complex sub-specialty surgeries. Many of our consultants have international reputations for their research in their specialised field.
Before your treatment
You will have a formal consultation with a healthcare professional. During this time you will be able to explain your medical history, symptoms and raise any concerns that you might have.
We will also discuss with you whether any further diagnostic tests, such as scans or blood tests, are needed. Any additional costs will be discussed before further tests are carried out.
Preparing for your treatment
We've tried to make your experience with us as easy and relaxed as possible.
For more information on visiting hours, our food, what to pack if you're staying with us, parking and all those other important practicalities, please visit our patient information pages.
Our dedicated team will also give you tailored advice to follow in the run up to your visit.
The procedure
We understand that having surgery can potentially be a time of anxiety and worry - even for a relatively straightforward procedure like this one. Our experienced and caring medical staff will be there for you, holding your hand, every step of the way.
Haemorrhoid removal treatment is usually performed under a general anaesthetic. This means you will be asleep throughout the operation.
Some people choose epidural anaesthesia instead. This numbs your body from the waist down, but you will still be awake.
We use a number of techniques for removing haemorrhoids:
Haemorrhoidectomy
A tight stitch (ligature) is placed around the base of the haemorrhoid to control any bleeding during the operation. Your surgeon will then make a cut on the outer part of the haemorrhoid and remove any excess tissue.
The wound may be closed with dissolvable stitches. Most of the stitches will be inside the anal canal and will dissolve over the course of about two to four weeks.
The surgeon may place an absorbent pack into your rectum to help stem any further bleeding. This usually stays in place until your first bowel movement. The operation usually takes between 30 and 60 minutes.
Circular stapled haemorrhoidectomy
A circular stapler is placed inside the rectum and removes a ring of the rectal tissue above the haemorrhoids. This blocks the blood supply to the haemorrhoids so that they shrink.
This is a fairly new technique, and the National Institute for Health and Clinical Excellence (NICE) has found that it works as well as the usual technique. There also seem to be fewer problems, such as bleeding afterwards.
Transanal Haemorrhoidal De-Arterialisation (THD) or HALO
THD - also called haemorrhoid ligation, haemorrhoidal artery ligation or doppler guided ligation - is an innovative, minimally invasive surgical procedure approved by NICE, which involves treating the piles by closing off the arteries that are feeding them. It is designed to cure them in a gentle way and provide excellent long term results.
The procedure does not involve cutting or removing any haemorrhoidal tissue, so minimises pain and reduces post-operative complications.
During THD, your surgeon will locate the haemorrhoid’s feeding arteries using an ultrasound Doppler probe mounted on a specially designed proctoscope (an instrument used to examine the rectum). He or she will then suture (close up with stitches) each of these arteries through an opening window in the proctoscope.
The procedure is carried out in an area without sensory nerves so you won't feel any stitches during or after it. THD treatment can also re-position prolapsed tissue (piles that are hanging down from your bottom).
The Transanal Haemorrhoidal De-Arterialisation (THD) or HALO procedure is not available at all Spire hospitals.
Rafaelo procedure
Using the safe and established technology of radiofrequency ablation, the Rafaelo procedure is performed as a short day-case procedure. It does not require a general anaesthetic and you will be able to return to your normal daily activities immediately after treatment. The Rafaelo procedure is designed to treat haemorrhoid grades 1–3. Some grade 4 haemorrhoids may be reduced but it is unlikely that they will not reach a complete resolution, which often will require surgery.
The Rafaelo procedure is not available at all Spire hospitals.
Watch a video about the Rafaelo procedure
The result may be a significant period of discomfort, itching and/or bleeding which we try to subtly cure with lotions and potions bought from the chemist – these might well settle the problem or may just temporise the symptoms for a while. If symptoms recur it may be advantageous to seek a medical opinion at an earlier stage to obviate the potential for more significant treatments further in time. Those of us who have suffered in the past, and who have undergone medical intervention, may recall an unpleasant experience – whether successful or not, often one which we would rather was not repeated.
Haemorrhoids are graded from 1 to 4. The small early ones might not have any symptoms or may cause itching or spots of blood when opening one’s bowels, to the larger and more external grade 4 external haemorrhoids for which surgery is the only option.
Grade 1–2 haemorrhoids can remain untreated, be monitored, and then perhaps be ‘banded’, were the symptoms to persist. Banding is a commonly used treatment to the early-grade haemorrhoids (grade 1 or 2) which entails the suction of the pile or the area just above it using a special implement and then attaching a small elastic band around the base. This effectively strangulates the pile, reducing its blood supply. It will subsequently fall away after a week or so, often unnoticed. The application of the bands, however, can be very painful, as can the strangulation process which follows. The bands may snap or fall off prematurely, which will require a further application but, more importantly, significant bleeding could result. Even if a banding application is initially successful, recurrence rates are high and one can expect to have a further application at some point in the future. If left to grow over time without seeking medical help, or failing to address dietary, toilet or lifestyle habits (which could improve the condition in the early stages), they may develop into more advanced grades.
From then on, if banding is no longer deemed suitable, more formal surgical procedures may be required for treatment. This may involve removing the haemorrhoidal tissue by surgical excision, which is a very painful procedure, for a few weeks until the wound/s have eventually healed. Most often this would require time off work, which may be up to 2–4 weeks. This brings us back to why some people avoid seeking treatment in the first place– they simply don’t want to go through the pain of the treatment, and it may not be convenient to take time off work. It can be a vicious circle! Remember, all grade 4 haemorrhoids were grade 1 at one point. What is ideally needed is a treatment that is safe and reliable with good long-term results, but which is minimally invasive, only takes a few minutes to perform, is less painful than some other existing options and doesn’t require time off work.
Aftercare
Haemorrhoid removal treatment is usually carried out as a day case procedure, so you won't usually need to stay overnight.
After this, you will be taken to your room or comfortable area where you can rest and recuperate until we feel you're ready to go home.
Pain relief
After a haemorrhoidectomy, you will have some pain at the site of the operation for a few days and there may be a small amount of bleeding or discharge from the anus.
Rafaelo is a quick day case procedure. Very little pain relief is required after the procedure, some people do take a couple of paracetamol for a day or two, but others don’t need any pain relief.
We will provide you with a supply of all the medicines your consultant feels you need to take home with you after you've been discharged, up to 14 days. This may be at an additional cost to some patients.
Recovery time
You may have some discomfort lasting for up to three weeks. Continue taking painkillers as advised by your healthcare team.
Follow your surgeon's advice about going back to work. You can expect to be off work for one or two weeks, depending on the nature of your job. Your surgeon will give you specific advice about when you can resume your normal lifestyle. You shouldn't do any heavy lifting, standing for long periods or strenuous exercise, but light exercise, such as walking, will help to speed up your recovery.
Most patients can expect to experience immediate cessation of their symptoms post Rafaelo procedure. Apart from possibly some slight bleeding within the first two weeks of treatment, there should be no other significant side effects.
How your loved ones can help
Once you're ready to be discharged, you'll need to arrange a taxi, friend or family member to take you home as you won't be able to drive.
Looking after you
Even after you've been discharged, we're still looking after you every step of the way. After haemorrhoid removal surgery, we will provide you with all the advice on what to do and not to do and the follow-up support you need.
Typically your consultant will want to see you after your treatment to see how you're doing. A follow up appointment will be made before you leave the hospital or clinic.
On rare occasions, complications can occur. If you experience any of these symptoms – constipation for a few days after the operation, you get a high temperature or fever, the amount of blood loss suddenly increases, you do not have a bowel movement for several days or you experience severe pain after a bowel movement, stitches coming apart, difficulty passing stools, bleeding that starts a week or more after surgery – call us straight away. Very occasionally, faecal incontinence, or a painful tear in the anus (fissure) can develop and further surgery may be needed.
The chance of complications depends on the exact type of procedure you are having and other factors such as your general health. Your consultant will talk to you about the possible risks and complications of having this procedure and how they apply to you.
If you have any questions or concerns, we're here to help.
To arrange your free mini consultation or to find out more:
Please call us on 0208 335 4646 or email:info@spirestanthonys.com
Why choose Spire?
We are committed to delivering excellent individual care and customer service across our network of hospitals, clinics and specialist care centres around the UK. Our dedicated and highly trained team aim to achieve consistently excellent results. For us it's more than just treating patients, it's about looking after people.
Important to note
The treatment described on this page may be adapted to meet your individual needs, so it's important to follow your healthcare professional's advice and raise any questions that you may have with them.
Procedures carried out at one of our Spire Healthcare Clinics will be performed under local anaesthetic.
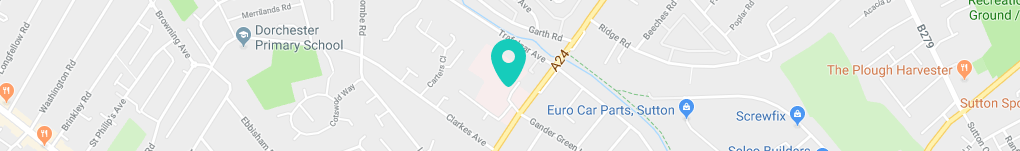
How to get to us
Spire St Anthony’s Hospital is a large private hospital providing an extensive range of treatments and services for our patients in Sutton and the surrounding Surrey and south London area.
Spire St Anthony's Hospital,
801 London Road
Cheam
Sutton
SM3 9DW
Get in touch
Important information about Covid-19 tests
COVID-19 testing or antibody tests are not available as a standalone service at Spire St Anthony's Hospital.